Evaluating Changes in Pulmonary Blood Vessel Shear Stress and Pressure Post-Pneumonectomy
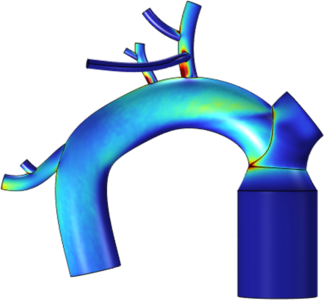
A pneumonectomy is an invasive, high-risk surgical procedure performed to remove the right or left lung. Although this may be a life saving procedure for some patients, it has high morbidity rates and many complications post-pneumonectomy. Pneumonectomies result in the heart’s entire cardiac output being directed into the remaining lung, which is believed to increase pressure and shear stresses within the remaining pulmonary vasculature. Changes in blood flow are sensed by the endothelial glycocalyx, a protective mechanotransduction layer on the endothelial cell layer of the blood vessels.[1] While the direct relationship between pneumonectomies and glycocalyx damage is not understood, there is a potential link between the blood flow changes created by pneumonectomies and the health of the glycocalyx. The increase in shear stress in the remaining lung’s vasculature following a pneumonectomy is speculated to cause damage to the glycocalyx at a faster rate than naturally repairable, which could contribute to postoperative complications and risks to the patient’s health.[2] This project attempted to create three virtual model variations of the pulmonary vasculature in SOLIDWORKS®: a control (no pneumonectomy version), and two pneumonectomy models, one per side. The two pneumonectomy models included the stump geometry remaining after the procedure. The 3D models’ geometry was limited to sparse literature found on morphology supplemented with FIJI data collection from a CT scan. The models were created to be very simple with cylindrical vasculature and did not include any elaborate or more realistic geometry for easier fluid flow simulation convergence. The three models’ geometry featured the main pulmonary artery, multiple vessels branching from the right and left pulmonary arteries, and individual vessel wall thicknesses assigned to each vessel supported by literature. Fluid flow simulations on these models were run in COMSOL Multiphysics® using the CAD Import Module to support the CAD geometry. The simulation was of a time dependent, laminar un-steady state flow. Piecewise functions determined a pulsatile-like flow environment. Specific pressures were defined at the inlet and outlets of each model as boundary conditions. A fluid-structure interaction was also used to study the interaction between the vessel walls and the fluid with material properties of blood. The laminar flow study used incompressible fluid flow. The results of the shear stress and pressure in specific areas of interest in the model at specific time steps were analyzed using MATLAB® to compare the control model with each pneumonectomy model separately. It was found that there was an increase in shear stress and pressure at certain bifurcations in the laminar steady state flow simulations as well as specific time intervals in the time dependent, laminar un-steady state flow simulations. These results are beneficial in understanding the environmental conditions the endothelial glycocalyx is under post-pneumonectomy and could provide research for post-operative complications.